About 2/3 of patients with IH report cognitive complaints (problems with thinking, reasoning, memory) and moderate to severe depression symptoms.1 IH is also linked with absence from work, inability to perform work duties while at work (presenteeism), and reduced ability to perform normal daily activities. These items can together reduce quality of life.1,2
There are several types of support for patients living with IH.
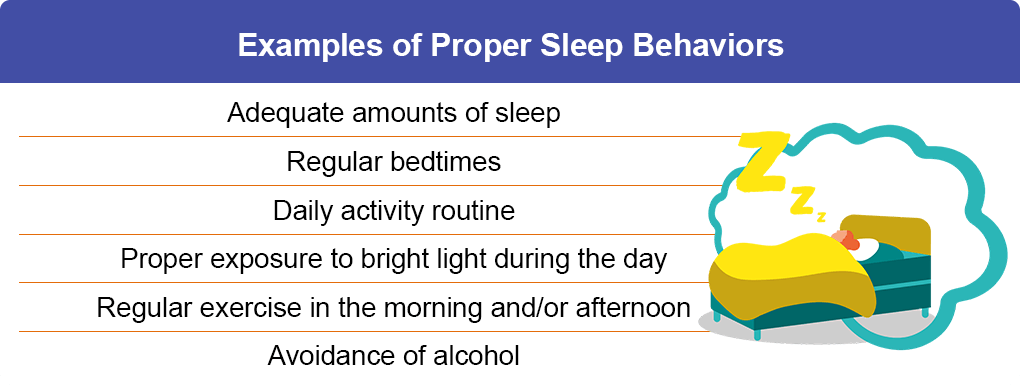
IH can be a difficult problem in daily life for those afflicted by it. You might notice that people close to you – family, friends, teachers, coworkers, etc – may mistake sleepiness for inattention or other emotions. Voice these concerns to your clinician; guidelines for IH recommend assessing and incorporating patient preferences and values when putting together a treatment plan. Your lifestyle and the cost of treatment should also factor in to initial and follow-up treatment decisions.2,3